CU Medicine invents a non-invasive technology for people with uninvestigated bowel symptoms
The Chinese University of Hong Kong (CUHK)’s Faculty of Medicine (CU Medicine) has, for the first time, discovered novel microbial signatures associated with inflammation of the gastrointestinal (GI) tract and transformed such signatures into clinically applicable non-invasive tests for early diagnosis and timely intervention. This invention can effectively differentiate common chronic gut disorders and is expected to minimise the need for endoscopies. Utilising nearly 6,000 faecal samples collected from different regions and ethnicities, the research team has developed the world’s first droplet digital polymerase chain reaction (ddPCR) test targeting selected unique bacterial species. This novel non-invasive diagnostic test is a reliable tool to differentiate irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD), and is expected to be ready for clinical use in 2027. The findings were published in Nature Medicine.

CU Medicine has, for the first time, discovered novel microbial signatures associated with inflammation of the gastrointestinal (GI) tract and developed the world’s first droplet digital polymerase chain reaction (ddPCR) test targeting selected unique bacterial species. This invention can effectively differentiate common chronic gut disorders and is expected to minimise the need for endoscopies. (From left) Professor Siew Ng, Croucher Professor in Medical Sciences, Director of the Microbiota I-Center (MagIC) and New Cornerstone Investigator; Professor Francis KL Chan, Choh-Ming Li Professor of Medicine and Therapeutics at CU Medicine, Director of the Centre for Gut Microbiota Research and Co-Director of MagIC; IBD patient Mr. Eric Lam; Dr Zheng Jiaying, Postdoctoral Fellow, and Professor Wendy Zhang Jingwan, Assistant Professor in the Department of Medicine and Therapeutics at CU Medicine.
Lack of a reliable, accurate, non-invasive test for IBD diagnosis
IBD, a growing GI disease in Asia, often shares similar symptoms such as recurrent abdominal pain and diarrhoea with IBS, which is a common functional GI disorder. Delayed treatment in IBD can lead to chronic inflammation of and ulcers in the digestive tract, and severe cases may require the removal of a damaged intestine or the creation of a stoma.
Professor Francis KL Chan, Choh-Ming Li Professor of Medicine and Therapeutics at CU Medicine, Director of the Centre for Gut Microbiota Research and Co-Director of Microbiota I-Center (MagIC), said: “Globally, over eight million people experience GI symptoms yearly and likely need endoscopies. Colonoscopy and histology with CT or MRI scans are commonly used for IBD diagnosis but there is not yet a reliable blood or stool test. The surge in demand for colonoscopies may result in long waiting times and delayed treatment. There is an urgent need for a non-invasive, accurate diagnostic test for IBD.”
Discovery of microbiome biomarkers for IBD diagnosis
The CU Medicine research team performed metagenomic sequencing of 5,979 faecal samples with or without IBD – ulcerative colitis (UC) or Crohn’s disease – from [1]11 countries, featuring different ethnicities. They identified microbiota alterations in IBD and uncovered 10 unique bacteria species associated with UC and nine associated with Crohn’s disease.
Dr Zheng Jiaying, Postdoctoral Fellow, Department of Medicine and Therapeutics, CU Medicine, said: “We found that IBD patients had more toxin-producing bacterial genes in the gut, such as Adherent-invasive E. coli and Proteus mirabilis, and they lacked a variety of bacterial species with anti-inflammatory functions.”
Professor Wendy Zhang Jingwan, Assistant Professor, Department of Medicine and Therapeutics, CU Medicine, added: “We constructed machine learning diagnostic models for IBD based on the novel bacterial markers and found that the models performed well in diagnosing ulcerative colitis and Crohn’s disease with an area under the curve of over 0.94.”

Mr. Lam says it took him one to two years to reach a diagnosis of Crohn’s Disease for his repetitive gastrointestinal symptoms. It was a very tough journey for him as he had to go through all sorts of examinations including blood tests, small bowel endoscopy and colonoscopy.
Transforming bacterial markers into a rapid, effective, clinically applicable innovation for IBD diagnosis
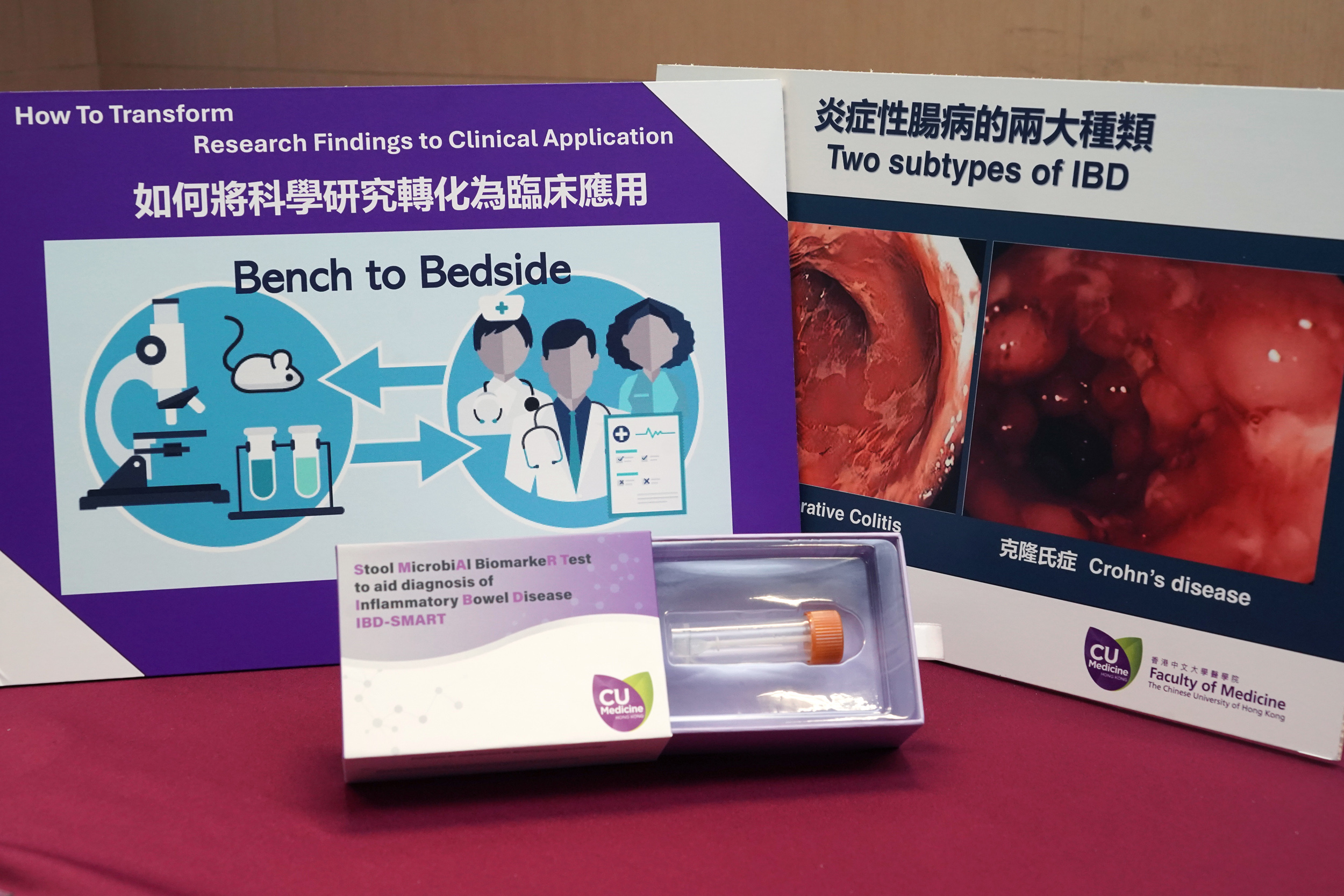
To transform the findings into clinical applications, the research team developed multiplex ddPCR technology to facilitate rapid, effective IBD diagnosis. Validation in independent cohorts and a public dataset showed a sensitivity of 88% and specificity of 89% for IBD diagnosis. The innovation has received national and international recognitions, including a Silver medal in the Geneva International Exhibition of Inventions 2024.
Professor Siew Ng, Croucher Professor in Medical Sciences, Director of the Microbiota I-Center (MagIC) and New Cornerstone Investigator, said: “The incidence of IBD is rising rapidly in Asia, and it is expected that the number of patients in China will exceed 1.5 million by 2025. CU Medicine has been a pioneer in the research of IBD diagnosis, treatment and prevention. We have now developed a first-in-class, microbiome-based, next-generation diagnostic tool for chronic intestinal diseases. We are also conducting large scale transethnic, multicentre studies to further explore the potential of these biomarkers in disease monitoring, drug response prediction and patient stratification in IBD.”
[1] 11 countries include US, UK, France, Spain, Germany, Austria, the Netherlands, Denmark, Japan, Australia and China (mainland and Hong Kong)