CUHK first discovers obese patients with diabetes and fluctuating blood glucose control had a high cancer risk while patients with diabetes treated with a common class of blood pressure lowering drug had a low cancer risk
Researchers at The Chinese University of Hong Kong (CUHK)’s Faculty of Medicine (CU Medicine) have reported two major findings related to cancer risk in patients with diabetes using big data. They first discovered that overweight or obese patients with diabetes and marked fluctuation in blood glucose control had 50% increased risk of cancer while patients with diabetes treated with renin-angiotensin-system inhibitor (RASi), a common class of blood pressure lowering drug, had a 50% lower risk of cancer. Findings have been published in medical journals The Lancet Regional Health - Western Pacific and EBioMedicine.
Diabetes affected 537 million people worldwide in 2021. In Hong Kong, one in eight adults have diabetes with a rising trend in young people. Diabetes and obesity frequently coexist to markedly increase the risk of critical illnesses including heart disease, stroke, kidney failure and cancer. With declining death rate from stroke and heart disease together with ageing, cancer is now one of the leading causes of death in people with diabetes. In Hong Kong, one in four patients with diabetes dies of cancer.

Researchers at CU Medicine have reported two major findings related to cancer risk in patients with diabetes using big data. They first discovered that overweight or obese patients with diabetes and marked fluctuation in blood glucose control had 50% increased risk of cancer while patients with diabetes treated with RASi, a common class of blood pressure lowering drug, had a 50% lower risk of cancer.
“Patients with suboptimal control of diabetes, especially in the presence of obesity, have an abnormal internal environment including low grade inflammation which can promote cancer growth. This partly explains the 30% to 300% higher cancer risk in patients with diabetes than in those without diabetes, especially liver, colorectal, pancreas, breast, and uterus cancers.”, said Professor Juliana Chan, Chair Professor of Medicine and Therapeutics at CU Medicine and Director of the Hong Kong Institute of Diabetes and Obesity.
The CUHK diabetes research team used real-world data from the Hong Kong Diabetes Register including 30,000 patients who were followed up at the Prince of Wales Hospital (1995-2019) and four million people who had ever had their blood glucose measured at public hospitals or clinics in the Hong Kong Diabetes Surveillance Database (HKDSD, 2000-2019) to discover emerging trends in diabetes and its complications in Hong Kong Chinese people.
Obese patients with diabetes and fluctuating blood glucose control have a 50% higher risk of any cancer than non-obese patients with steady blood glucose values
Glycated haemoglobin (HbA1c) is a percentage index of red blood cells in the body which are covered by glucose. For a normal range of blood glucose of 5-8 mmol/L, the corresponding HbA1c value is 5.0-6.5%. Since the oxygen-carrying red blood cells in the body are renewed every three months, HbA1c is used to measure the average blood glucose control during the same period.
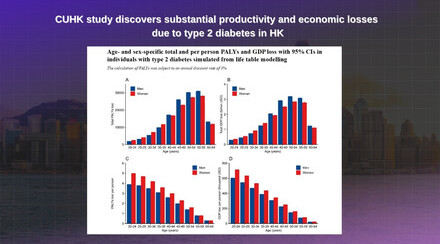
In 15,286 patients diagnosed with diabetes at an average age of 50 observed in 1995-2019, after having diabetes for 20 years, 928 patients developed cancer led by colorectal (n=184), liver (n=117) and breast (n=77) cancer, with 349 of them died with cancer. These patients had an average of 17 HbA1c measurements with 2-3 values every year. Researchers counted the number of HbA1c values measured during the observation period which varied by 0.5% compared with the previous value and expressed them as a percentage of the total number of HbA1c counts to indicate the level of fluctuation in blood glucose control (HbA1c variability score, HVS).
Stratified by a median value of 47%, the average HVSs in the high HVS and low HVS groups were 58% and 25% respectively. Compared to the low HVS group, the high HVS group had a 15% higher risk of developing any cancer. Obese patients (BMI ≥25 kg/m2) with high HVS had a 50% higher risk of any cancer especially of the breast (244%) and liver (263%) compared with non-obese patients with low HVS. These patients also had a 35-45% higher risk of death due to cancer, vascular and other causes including infection and kidney disease.
Lower risk of cancer in patients with diabetes treated with RASi a class of blood pressure lowering drug than non-users
In another analysis led by Dr Aimin Yang, Research Assistant Professor in the Department of Medicine and Therapeutics at CU Medicine, among 253,491 patients with type 2 diabetes, 5.9% were diagnosed with any cancer during 6.3 years of follow-up. They found that patients treated with RASi, a class of blood pressure lowering drug, had a lower risk of cancer than those not treated with RASi.
For the 47% new-RASi users, they had a 23% lower risk of any cancer and a 50% lower risk of cancer-related death than those not treated with RASi. Compared with non-users, amongst every 1000 RASi users, 2.6 all-site cancers, 6.3 all-cause deaths, and 2.2 cancer deaths were prevented every year. Compared with patients treated with another class of blood pressure lowering drugs, young patients treated with RASi also had a lower risk of cancer death.
Dr Elaine Chow, Assistant Professor in the Department of Medicine and Therapeutics at CU Medicine and senior author of the paper remarked, “High blood glucose, low grade inflammation and signals secreted from fat cells can activate angiotensin II (Ang II), a potent hormone which can increase blood pressure and stimulate cell growth. RASi reduces the activity of Ang II and has been confirmed to reduce the risk of heart disease, stroke and kidney failure in patients with diabetes. In the HKDSD, only 50% of patients were treated with this class of drug. Our novel data suggests that this drug class might lower cancer risk possibly by reducing the harmful effects of Ang II on cancer growth.”
These novel data emphasised the importance of good diabetes management with regular monitoring to avoid fluctuating blood glucose levels and obesity and as well as early use of organ-protective drugs such as RASi to reduce the risk of life-threatening events including cancer. This is particularly relevant to young people with diabetes, who face the prospect of suffering from the disease for a long time.
Professor Juliana Chan concluded, “Diabetes is a silent killer. Since 1995, CU Medicine has been a world pioneer in transforming the delivery of diabetes care by gathering data systematically and using the data to stratify risk, empower self-management and personalise care. These latest results highlight the impact of using data to influence policies and practices, and save patients’ lives.”
The study was supported by a CUHK Impact Research Fellowship Scheme, and other funding support.