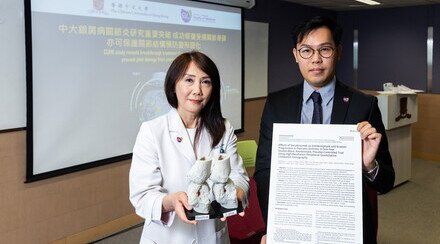
CUHK Pioneers the Use of 3D Echocardiography to Identify At-Risk Mitral Valve Prolapse Patients
A research team led by Professor Cheuk Man YU, Chairman, Department of Medicine and Therapeutics, Professor Alex Pui Wai LEE, Assistant Professor of Division of Cardiology and Professor Malcolm J. Underwood, Head of Division of Cardiothoracic Surgery, Department of Surgery at The Chinese University of Hong Kong (CUHK) pioneer the use of 3D (three-dimensional) echocardiography to identify at-risk mitral valve prolapse patients. The research team was the first to discover that the saddle shape of mitral annulus (ring) will become flattened in patients with mitral valve prolapse, making the mitral valve more susceptible to wear-and-tear, and predisposing a patient to develop mitral valve leaflet deformation, valve tendon rupture, and eventually severe mitral regurgitation. The findings have been published in the latest issue of the prestigious, international cardiovascular journal Circulation.

(From left) Professor Malcolm J. Underwood, Head of Division of Cardiothoracic Surgery, Department of Surgery; Professor Cheuk Man YU, Chairman, Department of Medicine and Therapeutics; and Professor Pui Wai LEE, Assistant Professor, Division of Cardiology at CUHK
Mitral valve is one of the heart valves and composed of two leaflets. When the mitral valve works normally, it keeps blood flowing from the left atrium (upper chamber) to the left ventricle (lower chamber). However, in mitral valve prolapse, one or both flaps do not close properly and mitral regurgitation may develop (in which blood flows back into the left atrium and lung). Mitral valve prolapse is present in about 3% of the general population, and among patients affected by this condition, about 7% will develop severe mitral regurgitation. Symptoms of mitral regurgitation include trouble breathing, tiredness, weakness, swelling in the ankles, legs, or belly, and even sudden death. These patients will need surgery to replace or repair their valves.
Traditional 2D (two-dimensional) echocardiography can only allow doctors to look at the heart in cross-sections. However, the mitral valve is a 3D and complex structure that moves rapidly in a beating heart. In order to obtain essential information for patient care, CUHK pioneers the use of 3D echocardiography to identify at-risk mitral valve prolapse patients by conducting a case-control study from year 2010 to 2012. A total of 112 subjects aged from 21 to 85 year-old, including 36 mitral valve prolapse patients who developed severe mitral regurgitation, 32 mitral valve prolapse patients with no or mild regurgitation, 12 patients with mitral regurgitation due to other causes, and 32 normal control subjects, were recruited for the study, having their mitral valve examined by 3D echocardiography. The investigators discovered that the fibrous ring (mitral annulus) that attached to the mitral valve is shaped like a 3D saddle. It helps relieve the forces exerted on the valve continuously by the constantly beating heart. The valve will degenerate quickly with its shape changed and components damaged under excessive wear-and-tear.

(From left) Professor Malcolm J. Underwood; Professor Pui Wai LEE and Professor Cheuk Man YU show the 3D Ultrasound System (Cardiology)
The research team made the first discovery that the saddle-shaped mitral annulus will become flattened in patients with mitral valve prolapse who developed significant mitral regurgitation, making the mitral valve more susceptible to wear-and-tear, and predisposing a patient to develop mitral leaflet deformation, valve tendon rupture, and eventually severe mitral regurgitation. The team also found that the chance of developing severe mitral regurgitation in patients with a flat mitral annulus is 7 times higher than those with a saddle-shaped mitral annulus. Twenty-four of the 36 (67%) mitral valve prolapse patients with severe regurgitation had a flat annulus, as compared to only 6 of the 32 (17%) patients with no or mild regurgitation; whereas among normal subjects and patients with regurgitation due to other causes, none of them had a flat annulus.
The results of the study will be useful to help doctors identify high-risk mitral valve prolapse patients, who should be monitored more closely by echocardiography. To avoid excessive wear-and-tear of the mitral valve, CUHK recommends to apply more aggressive measures to control blood pressure and body weight of high-risk patients.