CU Medicine leads new clinical practice guidelines on use of non-invasive biomarkers for colorectal cancer screening with international experts
The Chinese University of Hong Kong’s (CUHK) Faculty of Medicine (CU Medicine) led a team of a dozen international experts from the Asian Pacific Association of Gastroenterology and the Asian Pacific Society of Digestive Endoscopy in 2022 to develop new recommendations for the use of non-invasive biomarkers for colorectal cancer (CRC) screening. The findings have been published in high-impact international medical journal British Medical Journal – Gut.

CU Medicine leads new clinical practice guidelines on the use of “non-invasive biomarkers” for colorectal cancer screening with international experts. Non-invasive biomarkers have the potential to detect CRC and its precursor lesions and can allow risk stratification of suitable patients for colonoscopy.
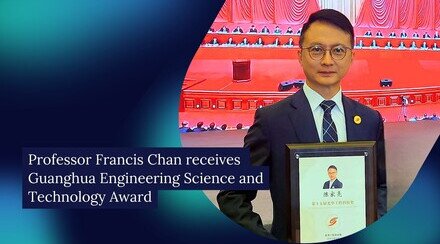
Research team members include (from left) Professor Siew Ng, CU Medicine’s Croucher Professor of Medical Sciences and Director of Microbiota I-Center (MagIC); Professor Francis KL CHAN, Dean of Medicine and Director of the Centre for Gut Microbiota Research; and Professor Martin Wong Chi-sang, Director of Centre for Health Education and Health Promotion and Professor from The Jockey Club School of Public Health and Primary Care at CU Medicine.
CRC is the second most common cancer in Hong Kong, constituting 15% of all new cancer cases in 2020. The incidence and mortality of CRC are expected to increase in the next few decades, leading to a significant public health burden. The incidence of and death rates from CRC can be reduced with CRC screening.
The Hong Kong government’s Department of Health has run a CRC screening pilot programme since 2016 but less than 15% of the eligible population have been tested to date. Reluctance to undergo colonoscopy and the suboptimal sensitivity of faecal immunochemical tests are key barriers to screening. Non-invasive biomarkers represent a novel method of CRC screening.
Non-invasive biomarkers can detect colorectal cancer with high sensitivity
Based on analysis of a systematic review of more than 800 medical articles, the research team recommends that the target population for non-invasive biomarkers for CRC screening should include:
- Individuals of average risk of advanced colorectal neoplasia identified by risk scores who wish to know their risk of adenomas and CRC
- Individuals at high risk of advanced colorectal neoplasia who are reluctant to undergo colonoscopy
Non-invasive biomarkers have the potential to detect CRC and its precursor lesions, and can allow risk stratification of suitable patients for colonoscopy. Current biomarkers for CRC screening include blood-based tumour biomarkers, stool-based tumour biomarkers and stool-based microbial biomarkers. Current blood-based biomarkers can only detect CRC and advanced adenomas with low sensitivity, while stool-based tumour biomarkers can be costly. Stool-based microbial biomarker tests have emerged as a significant improvement not only in the detection of CRC and adenoma, but also in their sensitivity in detecting recurrent adenomas and allowing for the potential of microbiota modulation to further reduce the risk of CRC.
Clinical application of stool-based biomarkers is promising and requires large-scale clinical studies in different populations for widespread implementation. CU Medicine is conducting a multi-centre clinical study in more than 10 countries to validate the findings regarding stool microbial biomarkers for CRC and adenoma detection.
Professor Francis KL CHAN, Dean of Medicine and Director of the Centre for Gut Microbiota Research at CU Medicine, said, “Detecting early precursor cancer lesions is important to reduce the CRC burden. Though the faecal immunochemical test (FIT) has been implemented for universal CRC screening, its diagnostic accuracy for detecting precancer lesions remains low. Its use in patients with iron deficiency anaemia or acute diarrhoea is not recommended. The new generation of stool-based and blood-based tumour and microbial biomarkers could increase the sensitivity of CRC diagnosis.”
Professor Martin Wong Chi-sang, Director of Centre for Health Education and Health Promotion and Professor in The Jockey Club School of Public Health and Primary Care at CU Medicine, said, “Clinical studies have shown that a combination of gut microbial makers composed of the novel Lanchnoclostridium gene marker (m3) has good diagnostic accuracy for both CRC and adenoma detection.”
Professor Siew Ng, CU Medicine’s Croucher Professor of Medical Sciences and Director of Microbiota I-Center (MagIC), added, “Emerging evidence suggests that the gut microbiota contributes to the development of CRC and adenomas. By identifying specific bacteria markers related to CRC, we hope to modulate the gut microbiome in high-risk individuals and reduce CRC risk. Maintaining a healthy gut microbiome is associated with many health benefits.”