CUHK study reveals daily prescription of 5mg of glucocorticoid doubles risk of cardiovascular events for patients with rheumatoid arthritis
Glucocorticoid is a potent anti-inflammatory drug used for prompt relief of synovitis symptoms, but its use remains controversial, as it increases the risk of cardiovascular disease.
The Chinese University of Hong Kong (CUHK)’s Faculty of Medicine (CU Medicine) conducted a long-term, population-based study to examine the time- and dose-dependent effect of systemic glucocorticoid on major adverse cardiovascular events (MACE) in patients with rheumatoid arthritis (RA). Results showed patients with RA who receive 5mg or above of glucocorticoid daily are at almost twice the risk of MACE. Researchers warned there is no safe duration of use at a daily dosage ≥5 mg and that the risk of MACE increases by 7% per month. Patients are advised to consult their rheumatologists about the possibility of tapering the dose of prednisolone to ≤4 mg daily if their joint symptoms improve. Alternatively, if necessary, they may consider early initiation of advanced therapy as a means to avoid the use of steroids. Findings have been published in the international journal Annals of the Rheumatic Diseases.

A CU Medicine study shows patients with rheumatoid arthritis (RA) who receive 5mg or above of glucocorticoid daily are at almost twice the risk of major adverse cardiovascular events (MACE). (From left) Mr. Tsang, patient with RA; Professor Tam Lai-shan, Head of Division of Rheumatology; and Dr So Ho,Assistant Professor in the Department of Medicine and Therapeutics at CU Medicine.
Debate over the use of glucocorticoid for patients with RA
RA is an inflammatory disease that causes pain, swelling, stiffness and loss of function in the joints. It occurs when the immune system, which normally defends the body from invading external organisms, turns its attack against body’s own tissue synovium (the membrane lining the joints) and causes inflammation. It is estimated that about 22,000 people suffer from RA in Hong Kong.

Professor Tam says patients with active RA should not arbitrarily reduce or stop the use of glucocorticoid due to the fear of increased cardiovascular risk. She suggests them following doctors’ instruction and seeking further medical advice when their disease activity index stabilizes.
Professor Tam Lai-shan, Head of Division of Rheumatology and Professor in the Department of Medicine and Therapeutics at CU Medicine, explained, “Glucocorticoid is widely prescribed at the initial presentation of active RA, as it shows an immediate effect in alleviating synovitis symptoms. However, the medicine may affect blood pressure, glycaemic metabolism and lipid profile, leading to an increased risk of cardiovascular disease. That’s why there have been debates over the use of systemic glucocorticoid on patients with RA who already bear a higher cardiovascular disease risk due to chronic inflammation. Both US and European advisory bodies in rheumatology review the clinical recommendations on glucocorticoid use from time to time.”
No safe duration of glucocorticoid use ≥5 mg for patients with RA
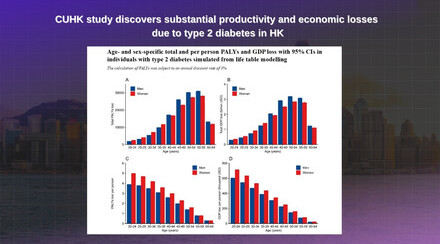
The CU Medicine research team recruited data from the Hospital Authority Data Collaboration Laboratory of 12,233 patients with RA who attended public hospitals between January 2006 and December 2015, with a mean follow-up duration of 8.7 years. None the patients had suffered from MACE, including myocardial infarction, unstable angina, ischaemic or haemorrhagic cerebrovascular incident, or transient ischaemic attack at the point when they were recruited. 37.7% of the patients were prescribed glucocorticoid at the study baseline, while other patients were put on alternative antirheumatic therapeutic options. The team found that the cardiovascular disease risk increased in a time- and-dose-dependent manner for patients with RA using glucocorticoid. Here are the key findings:
- There is no safe duration of glucocorticoid use ≥5 mg.
- A daily dose of glucocorticoid ≥5 mg results in a two-fold increased risk of MACE for patients with RA, and the risk rises by 7% per month of continued consumption.
- A low daily dose of glucocorticoid below 5mg does not appear to be associated with an increased cardiovascular disease risk.

Dr So says their research team will study the efficacy of glucocorticoid of 4mg or below in managing RA.
Dr So Ho, Assistant Professor of the Department of Medicine and Therapeutics at CU Medicine, said, “Our study provided answers to questions that had long been asked about dosage and duration tolerance of glucocorticoid use in patients with RA, and its cardiovascular risk. Based on our findings, we advise doctors to prescribe systemic glucocorticoid judiciously to patients with RA to balance the risks and benefits, and to discontinue or taper to less than 4mg daily as soon as possible.”
Professor Tam added, “We hope the findings send a powerful message to patients with RA who are still relying on glucocorticoid. Novel antirheumatic therapeutic options have emerged over the past 20 years, such as biological or targeted synthetic disease-modifying antirheumatic drugs, which are becoming more affordable and accessible.”

Mr Tsang has been suffering from RA for more than 20 years, with pain and stiffness in joints in the morning that he describes his hands as frozen chicken wings. He received glucocorticoid and immune-system suppressant as early treatment. In 2014, he was diagnosed with heart disease. He actively changed his living habits and was later switched to biological disease-modifying antirheumatic drug to control chronic inflammation. Both his RA and heart disease conditions are well managed.