CUHK reveals lifestyle intervention can alleviate metabolic dysfunction-associated steatotic liver disease in nearly 70% of people living with HIV
The Chinese University of Hong Kong (CUHK)’s Faculty of Medicine (CU Medicine) has conducted the first single-blind, randomised controlled clinical trial to assess the effectiveness of a dietitian-led lifestyle intervention programme in treating metabolic dysfunction-associated steatotic liver disease (MASLD) in people with human immunodeficiency virus (HIV). Nearly 70% of participants showed improvement in MASLD one year after such intervention, with significantly higher efficacy compared with that of standard clinical care, hence reducing the risk of developing severe liver disease and liver cancer in this high-risk population. Findings have been published in the prestigious journal The Lancet HIV.
Featured are (from left) Ms. Daisy Sin Man-ching, Assistant Lecturer, School of Life Sciences of CUHK and a registered dietitian; Dr Grace Lui Chung-yan, the -corresponding author of the study, Honorary Clinical Associate Professor from CU Medicine’s Department of Medicine and Therapeutics, and Consultant of PWH’s Department of Medicine and Therapeutics; Dr Li Guanlin, the first author of the study and Postdoctoral Fellow from Division of Medical Sciences, and Professor Vincent Wong Wai-sun, Mok Hing Yiu Professor of Medicine and Head of the Division of Gastroenterology and Hepatology, both from CU Medicine’s Department of Medicine and Therapeutics.
MASLD is a major cause of chronic liver disease in people with HIV. Its progression can lead to metabolic dysfunction-associated steatohepatitis (MASH) and even liver cancer. People with MASLD, other than having excessive liver fat (more than 5%), face risk factors such as being overweight and having high cholesterol. The condition of people with HIV and MASLD is much more likely to deteriorate compared with individuals without HIV. However, there has been a lack of randomised controlled clinical studies examining the impact of lifestyle modifications on resolving MASLD progression in these patients. As people living with HIV currently have limited pharmacological options for MASLD, more evidence-based clinical research is urgently needed to provide more tailored therapies for this population.
Researchers conducted a 12-month clinical study at the Prince of Wales Hospital (PWH) involving 84 people living with HIV and MASLD. Participants were aged 18 and above, on anti-retroviral therapy (ART) and had had HIV RNA of ≤50 copies per mL for at least six months. All participants, 88% of whom were male, were randomly assigned to either the intervention group or the control group. The intervention group participated in a dietitian-led lifestyle modification programme for one year, during which the dietitians followed standard procedures and advised on exercise and diet, such as standard dietary portions, and offered tailored health education on balanced nutrition and glycemic index. The control group received standard of care, including regular follow-up visits to assess HIV control, adherence to medications and management of comorbidities. Researchers then assessed whether participants’ liver fat dropped to less than 5%. Over 90% of participants completed all assessments post-intervention.
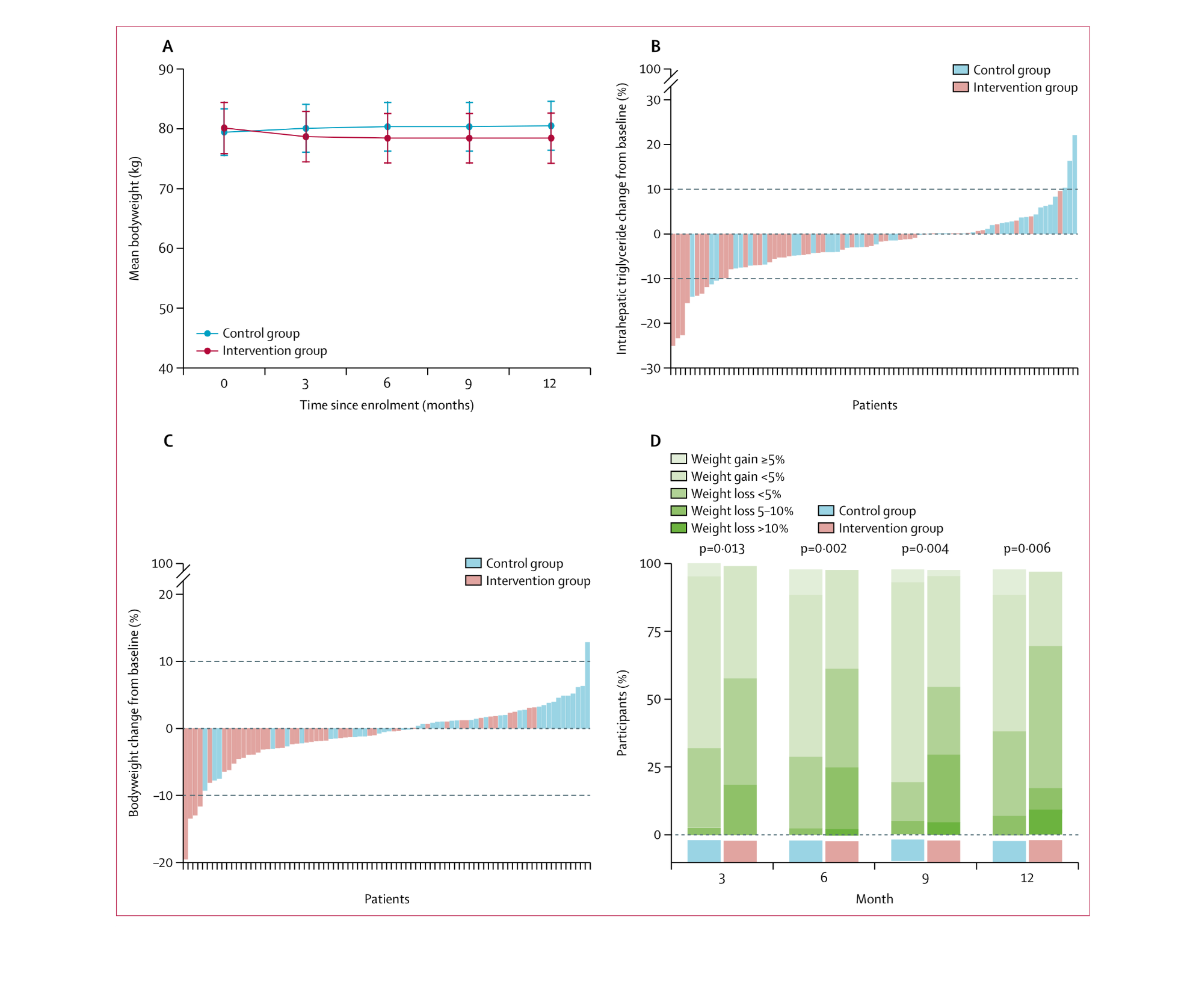
Having assessed the impact of lifestyle modification programme on participants’ bodyweight and BMI, researchers discover that the reduction of the mean bodyweight, intrahepatic triglyceride (liver fat) and individual’s bodyweight in the intervention group was more significant than that of the control group after one year, indicating more effective alleviation of MASLD with lifestyle intervention measures.
The results showed that 74% of participants in the intervention group saw improvement in MASLD, compared to less than 40% in the control group. The average decrease in body weight, BMI, total body fat, trunk fat and intrahepatic fat of the intervention group was also more than that of the control group.
| Resolution of MASLD in people living with HIV after the trial | Intervention group (43) | Control group (41) |
|---|---|---|
| Resolution of MASLD | 12 | 4 |
| Partial resolution of MASLD | 20 | 12 |
| % of the total number of participants in each group | 74% | 39% |
The main goal of lifestyle interventions is to improve health conditions by adjusting daily behaviours, such as modifying dietary habits and increasing daily physical activity. Dr Grace Lui Chung-yan, the corresponding author of the study, Honorary Clinical Associate Professor in CU Medicine’s Department of Medicine and Therapeutics, and Consultant in PWH’s Department of Medicine and Therapeutics, explained: “This study not only helps evaluate whether lifestyle interventions can mitigate MASLD in those with HIV but also provides valuable insights into key health indicators such as obesity metrics, inflammatory markers and liver fibrosis. Future studies should focus on analysing the efficacy of combining lifestyle intervention with pharmacological therapy, while exploring the potential for lifestyle intervention to be part of the routine treatment, expanding therapeutic options for HIV patients with MASLD.”
Professor Vincent Wong Wai-sun, Mok Hing Yiu Professor of Medicine and Head of the Division of Gastroenterology and Hepatology in CU Medicine’s Department of Medicine and Therapeutics, said: “MASLD affects over 30% of the global population. The pathogenesis of MASLD among people living with HIV is complex, with inflammation, behavioural factors and metabolic complication risks associated with ART contributing to it. The findings can provide more effective and tailored monitoring, interventions and treatment strategies for this population at higher risk of developing liver diseases, further reducing their risks of liver cancer and death.”
This study was supported by the Health and Medical Research Fund from the Health Bureau of the Government of the Hong Kong Special Administrative Region.