A major international study identifies biomarkers that enhance prediction accuracy of cardiovascular diseases in people with diabetes and have potential to change clinical practice
A major international collaborative study has identified 13 biomarkers that significantly improve the ability to accurately predict cardiovascular disease (CVD) risk in people with diabetes. They could potentially be used to enable clinicians to provide targeted advice and treatment to people with diabetes who are at most risk of developing CVD. The analysis, conducted by 23 experts from 11 countries, was led by The Chinese University of Hong Kong (CUHK) in Hong Kong, Johns Hopkins University in the United States and Lund University in Sweden. The findings have just been published in Communications Medicine, a publication of the Nature Group.
It is estimated that diabetes affected more than 500 million people worldwide in 2021. In Hong Kong, there are some 700,000 people with diabetes mellitus, which means one in every 10 people in the city has the condition, and the number is increasing sharply.
Although people with diabetes are twice as likely to develop CVD than those without it, it remains a challenge for clinicians to predict who among this population is most at risk. CVD is a major cause of hospitalisation and ill health among people with diabetes. While many biomarkers have been identified to predict the risk of heart disease, their utility among people with diabetes has not been well studied. Furthermore, it is necessary to evaluate whether these biomarkers provide better prediction of risk compared to current approaches.
Professor Maria Gomez, Professor of Physiology at Lund University Diabetes Centre and co-senior author of the study, noted, “Early identification of those at risk may facilitate early intervention and treatment. Our goal was to identify promising markers that could improve cardiovascular risk prediction in people with diabetes. We wanted to look beyond traditional prognostic factors like hypertension and smoking.”
“Our study team included 23 researchers from around the world. The study, conducted over more than three years, represents the largest and most ambitious overview of the state of knowledge on cardiovascular risk prediction in diabetes to date,” Dr Nestoras Mathioudakis, Co-Medical Director of Johns Hopkins Medicine Diabetes Prevention & Education Program, Associate Professor of Medicine at the Johns Hopkins University School of Medicine and co-senior author of the work, remarked.
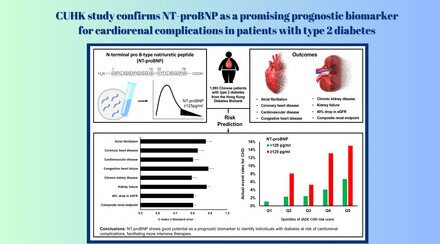
Researchers have undertaken a comprehensive review of more than 9,000 studies published from 1990 to 2021, to understand the most promising emerging candidates for prediction of CVD among people with diabetes and to investigate the differences between people with type 2 diabetes who experience CVD and those who do not. Out of the 195 biomarkers examined, the team found that 13 were significantly associated with CVD risk in people with type 2 diabetes. The most promising markers identified were N-terminal pro b-type natriuretic peptide (NT-proBNP), troponin-T (TnT), triglyceride-glucose (TyG) index and Genetic Risk Score for Coronary Heart Disease (GRS-CHD).
The standout biomarker was N-terminal pro b-type natriuretic peptide (NT-proBNP), a peptide currently used as a way to monitor heart failure status in patients. The team found that, across several studies, higher levels of NT-proBNP in the body correlated with a higher risk of CVD. One study of 16,000 patients that the team reviewed found a 64% hazard rate to develop CVD increase for every standard deviation increase of NT-proBNP.
“Our study highlights the potential for incorporating emerging biomarkers into clinical risk prediction and the potential for precision medicine in diabetes,” said Professor Ronald Ma, S.H. Ho Professor of Diabetes and Head (Academic Affairs) of the Division of Endocrinology and Diabetes at CU Medicine, and co-senior author of the analysis. “Future studies should systematically compare the different approaches in order to select the most promising approaches to risk stratification among people with diabetes. If their value in predicting cardiovascular risk in patients with diabetes is confirmed, we may be able to change standards of care.”
This study was conducted as part of the Precision Medicine in Diabetes Initiative (PMDI), an international partnership between the American Diabetes Association and the European Association for the Study of Diabetes. The main results of the study guided the recommendations of the Second International Consensus Report on gaps and opportunities for the clinical translation of precision diabetes medicine, which was published recently in Nature Medicine, and represented a collaborative effort from more than 200 researchers from 28 countries. The full Consensus report is available here: