CUHK proves the eHealth App’s Health Management module helps promote self-management of diabetes
The Chinese University of Hong Kong’s (CUHK)’s Faculty of Medicine (CU Medicine) and the Health Bureau have conducted a study to evaluate the effectiveness of the eHealth App, an electronic mobile health application, in self-management from patients with diabetes. Results showed the app’s Health Management Module generated satisfactory outcomes in blood sugar control among patients with diabetes, especially young female users. Findings have been published in npj Digital Medicine, a medical publication under Nature.
App’s health management function enhances patients’ management of their own health and promotes communication with medical workers
The government launched eHealth App in January 2021 as a free, user-centric public health hub with one-stop access to health information. It added a Health Management Module in July of the same year, where users could record and manage blood pressure, blood sugar and heart rate for themselves and their families. Doctors and nurses can provide more holistic care for these patients after assessing this real-time health information.
Previous literature has suggested that mobile applications positively impact diabetes self-management. CU Medicine and the Health Bureau rolled out a study to examine how effectively the eHealth app could do so.
The Health Management module facilitates diabetes management, but use remained low among older people
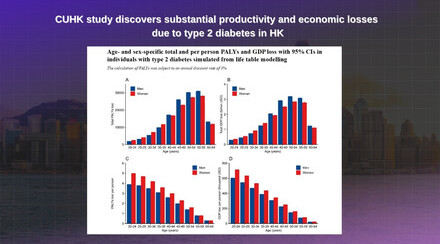
CU Medicine and the Health Bureau collected and analysed data from 109,823 patients with diabetes between January 2021 and May 2022 to assess the association of different factors with the optimal HbA1c level (lower than 7%). The factors included demographics, lifestyle, HbA1c level and use of the eHealth app and its Health Management module. 31,723 study participants were eHealth app users, 1,744 people used both the app and its Health Management module, and the remaining 76,356 patients were not eHealth app users.
Results showed eHealth app use is positively associated with optimal HbA1c levels, and patients who used the Health Management module had the best blood sugar control. The tendencyof patients who could attain the optimal HbA1c level is 40% higher in the Health Management module group than among non-eHealth app users. That figure jumped to 60% among young female Health Management module users. The research team also observed low use of the eHealth app among older people, with only 24% of patients aged 60 or above using it, compared to close to half of those aged under 60 (43%).

Dr Jason Huang says a low use of the eHealth app was observed among older people aged 60 or above and he encourages their family members to use eHealth to help manage their health.
Dr Jason Huang Junjie, the first author of the study and Research Assistant Professor of the Jockey Club School of Public Health and Primary Care at CU Medicine, said, “We found that patients with diabetes who are using eHealth and its Health Management module performed the best in controlling HbA1c levels, especially the young female group. Reasons could include that they are more concerned about their health than other groups and actively seek health information, and that they are more familiar with mobile applications. It is very important for elderly people with diabetes to control their blood sugar to an optimal level. We should think about ways to help them overcome the technical barriers in using the eHealth app, and encourage their family members to use eHealth to help manage their health.”

Professor Martin Wong says the research team plans to conduct a large-scale clinical study to further evaluate the different parameters in the eHealth app including blood pressure, blood sugar level in promoting self-health management for patients with diabetes.
Professor Martin Wong Chi-sang, senior corresponding author of the study and Professor of the Jockey Club School of Public Health and Primary Care at CU Medicine, added, “This study validated the potential of the eHealth app and its health management functions for diabetic patients. Another advantage of eHealth is that it enables medical staff in public and private hospitals in Hong Kong to monitor patients’ blood sugar records in real time with the patient’s consent, helping to provide more timely diagnosis and treatment. We recommend strengthening promotion of the eHealth app and its health management functions to patients with diabetes, so that they can manage their health better.”
The original study can be accessed here: https://www.nature.com/articles/s41746-023-00807-w