CU Medicine Studies Highlight Smoking as a Contributing Factor for Bladder Cancer and Develop an International Collaborative Consensus on En Bloc Resection to Treat the Disease

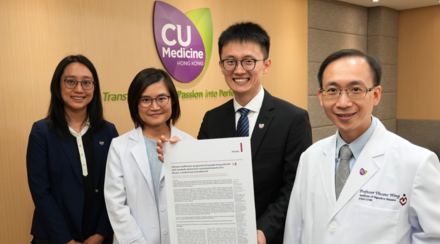
CU Medicine has recently published two studies on bladder cancer, in both epidemiology and treatment aspects, in the prestigious international urological journal European Urology. (From left: Professor Martin Chi Sang WONG, from The Jockey Club School of Public Health and Primary Care; Assistant Professor Dr. Jeremy Yuen Chun TEOH and Professor Anthony Chi Fai NG from the Division of Urology, Department of Surgery at CU Medicine)
Bladder cancer is a major urological disease and among the top 10 most common cancers in the world. The Faculty of Medicine of The Chinese University of Hong Kong (CU Medicine) has recently published two studies on the disease, in both epidemiology and treatment aspects, in the prestigious international urological journal European Urology. The first study reviewed the global trends of bladder cancer incidence and mortality, also their associations with smoking and financial capacity. In the second study, CU Medicine developed an international collaborative consensus statement on the use of en bloc resection for the treatment of bladder cancer.
Bladder cancer targets the older population and with high recurrence rate
Bladder cancer is the top 10th most common cancer in the world with approximately 550,000 new cases being diagnosed every year. In Hong Kong, there are about 400 new cases every year, commonly diagnosed in people aged between 55 and 70. Most bladder cancers are diagnosed at an early stage with the commonest presentation being blood in urine without any pain.
Professor Anthony Chi Fai NG, from the Division of Urology, Department of Surgery at CU Medicine and Director of S.H. Ho Urology Centre at CUHK said, “Bladder cancer is seldom mentioned in Hong Kong compared with lung, breast or colorectal cancer because it’s not among the top 10 cancer types in Hong Kong. However, given that it is a disease targeting the older population and that it recurs particularly easily, we believe it is equally important to study the disease, in both epidemiology and treatment aspects to provide better patient care.”
Smoking as a major contributing factor to bladder cancer globally
CU Medicine team led an international collaborative research that studied the global trends of bladder cancer incidence and mortality, and also their associations with smoking and financial capacity. Researchers retrieved data from various sources including the Global Cancer Observatory (GLOBOCAN) database, the Cancer Incidence in Five Continents released by the International Association of Cancer Registries (IACR) and the World Health Organization (WHO) database. A summary of the major findings in global incidence and mortality trends of bladder cancer is as follow:
- The 10-year temporal trend study showed an increase in incidence rate but a decline in mortality rate for bladder cancer in European countries. In Asia, on the contrary, it showed a decreasing incidence rate but increasing male mortality rate.
- Among countries with a decreasing smoking trend and, a higher financial capacity there was a further reduction in the bladder cancer mortality rate
Professor Martin Chi Sang WONG, corresponding author of the study, from The Jockey Club School of Public Health and Primary Care at CU Medicine said, “We observed wide variations in bladder cancer incidence and mortality rates globally. This can be possibly explained by a better awareness and earlier detection of the disease in European countries, resulting in better oncological control and reduction in the mortality rate. However, in most Asian developing countries, many people may have limited access to public health services, resulting in a lack of access to more advanced oncological treatment that has a long-term effect on cancer control. The ageing population in the region further increases the urgency for a better allocation of health care resources.”
Another key area of investigation is whether smoking serves as a contributing factor to bladder cancer. Results showed there is a positive correlation in both incidence and mortality for male and female.
Male (age-standardised rate) | Female (age-standardised rate) | |
|---|---|---|
Coefficient of Correlation between the rate of tobacco use and bladder cancer incidence | 0.20 | 0.67 |
Coefficient of Correlation between the rate of tobacco use and bladder cancer mortality | 0.38 | 0.22 |
Professor WONG explained, “Tobacco contains a rich source of harmful carcinogenic compounds which may accumulate in the urine and damage the lining of the bladder, increasing the risk of cancer. Earlier international study has already suggested smoking is the most important risk factor for bladder cancer, with an attribute risk of about 50%. It might also affect the progress of bladder cancer.”
Professor Anthony NG added, “When we educate the public about prevention for bladder cancer, the number one rule is ‘don’t smoke’. The WHO has set a global target of a 30% relative reduction in the prevalence of tobacco use in persons aged 15 or above by 2025. Hopefully a global effort to stop smoking would help reduce the burden on bladder cancer care in the long run. Among with that, maintaining a healthy lifestyle, drinking more water or having more fruits and vegetables that are rich in antioxidants may help reduce the risk of cancer.”

Professor Martin WONG says they have observed wide variations in bladder cancer incidence and mortality rates globally. A better oncological control and reduction in the mortality rate of the disease was present in Europe compared to Asia. Given that bladder cancer is a disease targeting the older population, the ageing population in the Asian region further increases the urgency for a better allocation of health care resources.

Professor Anthony NG says smoking cessation, maintaining a healthy lifestyle, drinking more water or having more fruits and vegetables that are rich in antioxidants may help reduce the risk of bladder cancer.
International Consensus On the Use of En Bloc Resection of Bladder Tumour
Depending on the stage of cancer and other factors, treatment options vary among patients with bladder cancer. They include surgery, chemotherapy, radiation therapy, immunotherapy, intravesical therapy and targeted therapy drugs. Surgery is part of the treatment for most bladder cancers and the type of surgery depends on the extent of the cancer.
Transurethral resection of bladder tumour (TURBT) is the most common conventional method for early-stage non-muscle invasive bladder cancers. It involves piecemeal resection of the tumour to remove the cancer cells and nearby tissues down to the muscle layer of the bladder wall. Yet, TURBT has a very high recurrence rate, and if it does recur, repeated surgery has to be performed. In the last decade, urologists have been exploring en bloc resection of bladder tumour (ERBT) as a potentially superior alternative to TURBT. This novel method which emerged in the 1980s allows resection of the tumour in one piece for better histological assessment of the resection margins and also avoid tumour fragmentation and minimises the risk of tumour recurrence. As the process is more precise and controlled, it also has a lower risk of bladder perforation.

Dr. Jeremy TEOH says en bloc resection of bladder tumour allows resection of the tumour in one piece and avoid tumour fragmentation, thus minimising the risk of tumour recurrence.

Dr. TEOH explains the procedure of en bloc resection of bladder tumour.
Dr. Jeremy Yuen Chun TEOH, Assistant Professor from the Division of Urology, Department of Surgery at CU Medicine said, “Although urologists are aware of the advantages of ERBT in treating bladder cancer, there is a lack of recommendations of this surgical procedure globally. Therefore, CU Medicine has carried out the most comprehensive review of scientific evidence on the treatment, and led the development of a consensus statement on ERBT by a two-round Delphi survey involving more than 100 health care professionals with experience in ERBT and an expert consensus meeting to define various important aspects of ERBT. Finally, a total of 99 statements reached consensus and they will be served as a standard reference for the urological community in the future.”
Summary of the major findings is as follows:
- ERBT is a new approach for treatment of non-muscle-invasive bladder cancer, and may have a better clinical outcome than the traditional approach
- ERBT is feasible for bladder tumours smaller than 3cm, and even for bladder tumours larger than 3cm
- Quantity and location of bladder tumours are not the major limitations in performing ERBT
- The main goals of ERBT are to ensure complete local resection and to reduce the risk of tumour reimplantation
- ERBT has a lower rate of bladder perforation than conventional TURBT
“The consensus statement will provide guidance for health care professionals who practise ERBT and inform researchers regarding ERBT-related studies in the future. Treatment for bladder cancer depends on its type, patients’ medical history and their personal preferences. Therefore we suggest patients have a thorough discussion with their doctors on the best treatment option,” Dr. TEOH added.

Mr. YEUNG found blood in urine in 2017 and was later diagnosed with bladder cancer. He received en bloc resection to remove the tumour and had no adverse effects.