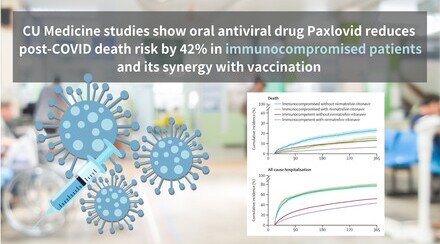
CUHK study shows oral antiviral drug Paxlovid can reduce the risk of post-acute death and sequelae among hospitalised COVID-19 patients
The Chinese University of Hong Kong (CUHK)’s Faculty of Medicine (CU Medicine) conducted a retrospective investigation using real-world data to examine the association of Paxlovid (also known as nirmatrelvir-ritonavir) with post-acute sequelae in hospitalised COVID-19 patients, as well as mortality. The results showed that the risk of post-acute inpatient death (i.e. death occurring 21 days after a positive test result) in COVID-19 patients who were hospitalised and prescribed oral Paxlovid within five days after symptom onset was significantly reduced by 38% compared to those who were hospitalised and didn’t use the drug during the acute phase. Similar effects were observed on the post-acute sequelae of cardiovascular and respiratory complications. Study results have been published in the journal The Lancet Infectious Diseases.
Study results showcase the long-term benefits of antiviral drugs against COVID-19
The literature suggested that the prevalence of post-COVID-19 conditions among individuals infected with SARS-CoV-2 may range from 10% to 30%. Despite authorised use of Paxlovid for treating COVID-19 in late 2021, few investigations have evaluated the association of the drug with post-acute sequelae and mortality, especially in hospitalised patients.
The current study used the real-world COVID-19 surveillance data obtained from Hong Kong Hospital Authority and Department of Health. The research team analysed more than 50,000 hospitalised COVID-19 patients aged 18 and over in Hong Kong between March 2022 and October 2023. Among them, approximately 15,000 were prescribed Paxlovid within five days of symptom onset, while those who did not take the oral drug during the acute phase were grouped as the control.
Study findings revealed that the risk of post-acute death of hospitalised COVID-19 patients who were prescribed oral Paxlovid was 6.9%, which is lower than the 13.5% risk of those hospitalised who did not use the drug. The reduced risk is 38% after adjusting for their demographics, clinical background and vaccination status. Similar effects were observed on the post-acute sequelae of cardiovascular and respiratory complications. Details can be found in table 1 in the appendix.
Professor Marc Chong Ka-chun, a corresponding author of the research paper and Assistant Professor at The Jockey Club School of Public Health and Primary Care of CU Medicine, said, “Public health agencies should adequately prepare effective antivirals to manage both acute and post-acute conditions of COVID-19, particularly considering the ongoing emergence of new variants of concern of the SARS-CoV-2 virus.”
Professor Yeoh Eng-kiong, also a corresponding author of the research paper and Director at the Centre for Health Systems and Policy Research at CU Medicine’s The Jockey Club School of Public Health and Primary Care, stated, “To our knowledge, our study is the first to highlight the extended benefits of Paxlovid in patients admitted to hospital with COVID-19. This study showcases the long-term benefits of the antiviral serving as a valuable complement to COVID-19 vaccines in mitigating the global clinical burden of COVID-19 in the years ahead.”
The research team member included Ms Wang Hu-wen, a doctoral student from The Jockey Club School of Public Health and Primary Care at CU Medicine. Ms Wang was one of the awardees of the Research Grants Council’s Hong Kong PhD Fellowship Scheme 2021/22 and is the first author of the published paper.
The study was supported by the Health and Medical Research Fund and other funding.
The full study can be accessed at: https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(24)00217-2/fulltext.
Appendix
Table 1: The effect of Paxlovid on the risks of post-acute sequelae of COVID-19 and mortality from the disease
| Percentage of patients with the respective post-COVID sequelae |
| |
Control | Patients prescribed Paxlovid | *Reduced risk of patients prescribed Paxlovid | |
Death | 13.5% | 6.9% | 38% |
Congestive heart failure | 2.4% | 1.5% | 30% |
Atrial fibrillation | 2.3% | 1.4% | 37% |
Coronary artery disease | 2.5% | 1.7% | 29% |
Chronic pulmonary disease | 1.7% | 1.1% | 32% |
Acute respiratory distress syndrome
| 2.7% | 1.3% | 29% |
End-stage renal disease | 0.2% | 0.1% | 63% |
* Figures adjusted for study participants’ demographics, clinical background and vaccination status.