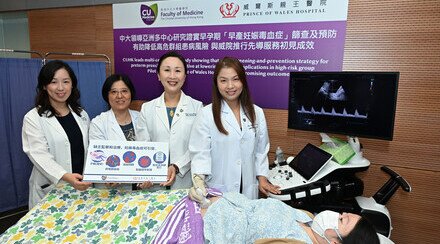
CU Medicine Study Shows Recovered Mothers Transfer COVID-19 Antibodies to Newborn Babies
A recent study led by the Department of Obstetrics and Gynaecology of The Faculty of Medicine at The Chinese University of Hong Kong (CU Medicine) showed that babies born to mothers who have recovered from COVID-19 infection have antibodies against the virus. The study, which has been published in Ultrasound in Obstetrics and Gynecology, also demonstrated that anti-SARS-CoV-2 Immunoglobulin G (IgG) concentrations in cord and maternal sera at delivery were highly correlated.
12 of 13 neonates born to mothers with recovered infection have antibodies
The CU Medicine team and its counterparts, which include the Obstetrics and Gynaecology Department from eight public hospitals in Hong Kong (Prince of Wales Hospital, Queen Elizabeth Hospital, United Christian Hospital, Princess Margaret Hospital, Tuen Mun Hospital, Kwong Wah Hospital, Pamela Youde Nethersole Eastern Hospital and Queen Mary Hospital), participated in this study. They recruited pregnant women with SARS-CoV-2 infection between March 2020 and January 2021, and analysed data from 20 subjects who had delivered their babies by 31 January 2021.
7 of them were with active infection or did not produce antibody by the time of delivery. 12 of 13 neonates born to mothers with recovered infection tested positive for IgG. All neonatal nasopharyngeal swab samples were reported to be negative for SARS-CoV-2 and all cord sera tested negative for Immunoglobulin M (IgM), meaning the neonates were not infected with the coronavirus.
Professor Liona POON, the key investigator of the study and Professor from the Department of Obstetrics and Gynaecology at CU Medicine said, “There is emerging evidence showing that if a woman is infected with SARS-CoV-2 during pregnancy, it is possible for her baby to pick up immunity to the virus in the womb. In this study, we confirmed the mother-to-child transfer of anti-SARS-CoV-2 antibodies and realised that the median transplacental transfer ratio of anti-SARS-CoV-2 IgG was 1.3, which means newborns have 30% higher levels of anti-SARS-CoV-2 IgG concentrations than their mothers.”
The higher the viral load of the mother, the lower the transplacental IgG transfer ratio
The study also brought in an additional dimension regarding the effect of viral load on transplacental IgG transfer. Here are the key observations:
- There was a positive correlation between IgG concentrations in maternal sera with viral load.
- A negative relationship was observed between IgG concentration in cord and maternal sera with infection-to-delivery interval — meaning the longer the interval the lower the IgG concentrations.
- There was a significant negative relationship between the transplacental IgG transfer ratio with viral load.
“Despite the high viral load leading to higher concentrations of anti-SARS-CoV-2 antibodies in affected mothers, it affects the transplacental transfer of IgG to the fetuses. Antibody transfer from the mother to the fetus depends on the maternal antibody levels, antibody receptors in the placenta and glycosylation profiles of the antibody. As in other infections, we observed that in maternal SARS-CoV-2 infection, neonatal antibody levels are proportional to maternal antibody levels. But maternal SARS-CoV-2 viral load restricted the transplacental IgG transfer. Possible explanations include alteration of antibody receptors in the placenta or glycosylation profiles of the antibody as shown by other researchers. Our findings raise the question of the potential impact of vaccine-induced immune response on mother-to-baby transfer of anti-SARS-CoV-2 IgG. There is an urgent need to generate clinical data on efficacy and safety of the various COVID-19 vaccines in pregnant women as well as to determine the vaccine technology and timing of vaccination which can best deliver maximum potential benefits to pregnant women and their babies,” she added.

The Obstetrics and Gynaecology Department of CU Medicine and its counterparts from eight public hospitals in Hong Kong participated in a study which showed that babies born to mothers who have recovered from COVID-19 infection have antibodies against the virus. It also demonstrated that anti-SARS-CoV-2 Immunoglobulin G (IgG) concentrations in cord and maternal sera at delivery were highly correlated.