A CU Medicine-Baylor College of Medicine collaborative study reveals for the first time that variations in DHX9 underlie human neurodevelopmental disorders
Neurodevelopmental disorders represent a spectrum of diseases, from mild to severe, that affect brain functions and neurological development. Some common examples include autism spectrum disorder, attention deficit hyperactivity disorder (ADHD) and intellectual disability. These developmental issues are estimated to affect 15-20% of children, making them a prevalent concern during childhood and adolescence worldwide.
Due to an increasing amount of evidence linking defects in DHX genes to neurodevelopmental disorders, an international team of researchers from The Chinese University of Hong Kong (CUHK)’s Faculty of Medicine (CU Medicine), Baylor College of Medicine and the German Mouse Clinic collaborated on a study of the pathogenesis of patients with neurodevelopmental disorders. The research team revealed for the first time that pathogenic variants in DHX9 disrupted the gene’s normal function. Further study using cellular and animal models supported the conclusion that defective changes in DHX9 underlie human neurodevelopmental problems. This is the first time that this gene has been associated with a human disease. The findings have been published in the American Journal of Human Genetics.
Study looks at neurological diseases from a genetic and genomic variation viewpoint
DHX9 encodes a helicase, an enzyme that plays a critical role in many cellular processes, including regulating DNA replication and RNA transcription, and maintaining genomic stability. Dysregulation of these processes is involved in disease mechanisms that result in neurodevelopmental disorders. The research team provided a genetic diagnosis to a group of 20 patients with undiagnosed neurodevelopmental disorders ranging from severe to mild, all with pathogenic changes to this gene.
To understand how patient-specific variants of the gene can cause defects, the team conducted cell-based functional studies. Cellular studies demonstrated that pathogenic DHX9 variants could modify the subcellular localisation of its expressed protein, increase genome instability and, in some cases, alter helicase ATPase activity, which are all key functions of the gene.

Professor Linda Gu Shen, Assistant Professor of the School of Biomedical Sciences at CU Medicine and the co-corresponding author of the publication, said, “These cellular studies allowed us to distinguish quite clearly the functional alterations in the variants in severe cases from those associated with less severe or the mildest cases. Their molecular pathogenic mechanisms could be different.”
Professor Albert Cheung Hoi-hung, Assistant Professor of the School of Biomedical Sciences at CU Medicine and one of the senior authors of the publication, said, “The biological functions of many DNA and RNA helicases remain to be characterised. Most importantly, the different pathogenic DHX9 variants were clearly seen in patients. Future research will rely on animal models and human organoid models to study the disease mechanism.”

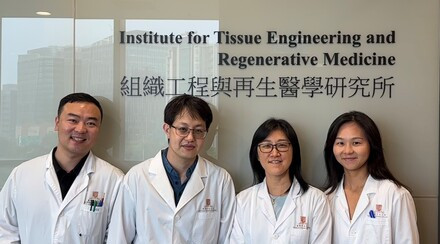
Researchers from CU Medicine include (back row, from left) Assistant Professor Albert Cheung Hoi-hung, Assistant Professor Linda Gu Shen and PhD. Student Ms. Cheryl Chen Wang; (front row, from left) research assistant Ms. Lily Liu Lingxiao and PhD. student Ms. Ava Guo Tianyu from the School of Biomedical Sciences at CU Medicine.